Interview SLU Alumnus Martin Pelletier, a Paramedic During COVID-19
Thao Nguyen (TN): Hi Marty, this is Thao from The Hill News. For the record, can you first introduce yourself to the readers who you are and what you’re doing during this COVID-19 outbreak?
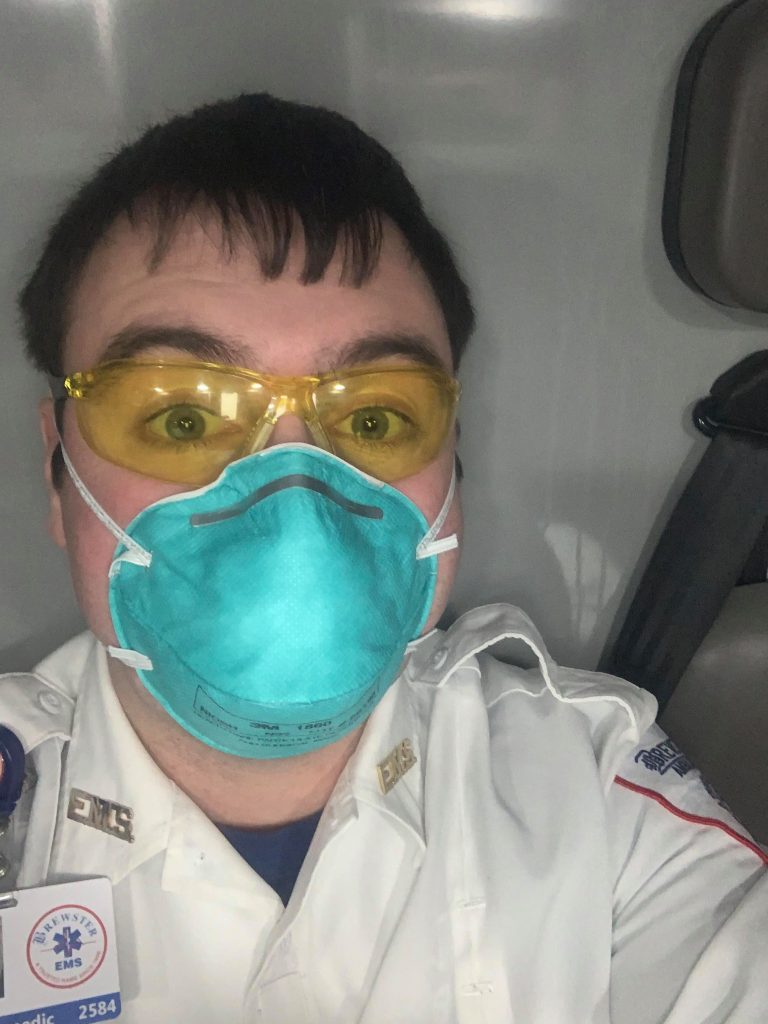
Marty Pelletier (MP): Yes. My name is Martin Pelletier, a St. Lawrence University alumnus of 2018. After graduation, I continued my job as a paramedic in the greater Boston area. I’ve been working there while working on other post-graduation plans. However, as we all know, the pandemic struck this February and March in the whole country, including my area of the Greater Boston. So, I work with Brewster Ambulance as a paramedic and I’ve encountered these patients in various instances.
TN: Thank you. Again, we just want to say thank you for all your hard work during this time. Yeah, so we just want to know how are you this day? Also, is your job much different now than it normally is?
MP: Right now, it’s different in a sense that there’s a lot of unknowns. This is the first time I’ve experienced a pandemic, obviously. That’s so we are now constantly having to put on personal protective equipment (PPE). About every time we work with patients, we have our masks on, be just regular patients. But you assume that everyone has it and you protect yourself the best you can. You also have to mentally prepare yourself since the virus itself is very infectious. It’s important to remind yourself before going to work about what the worst-case scenarios. Honestly, that is very anxious for some. But I’ve learn using your equipment and your training properly, you will be just fine.
TN: Yeah, definitely. I imagine that you and your coworkers are asked to show up to work because you’re the paramedics during this time, but there are still underlying worries about getting sick or not having enough time for your family. So, do you guys have enough people?
MP: Yes, right now we have very good staffing. Yet I know it’s not the same, you know, in other areas. It’s not surprising that we are encountering shortage of essential workers in regions such as New York City.
TN: Yeah. So, do you do you guys prepare for a possibility of not having enough people to work during the pandemic?
MP: Do we have enough people? I don’t know the details behind it, but what I do know is we have a strong pool of paramedics where I work at Brewster ambulance. We have full time and also some part time nurse as well. They do fill in the gaps pretty well. But I don’t know the details yet. What I can say is the state of Massachusetts has prepared for it. For the people who were EMTs or paramedics in the past now have the opportunity to recertify again to renew their certifications. Some of the restrictions on passing the requirements for the time being has been lifted.
TN: That’s really great to hear. Yeah, I think I would like to hear more about a day’s work that you’re doing
MP: That will involve coming in, whenever it starts in the morning or that evening, getting in early, and getting the reports from the off, going through how their shift was, what the stuffs we need are because there’s a lot of equipment on board. And then after getting my stuff together my gear, I will work on checking out trucking. I will look over the truck, mechanically, equipment wise, doing that sort of thing. And then, inevitably during that time maybe during the check or afterwards, this is why it’s important for people to continuously maintain, because we can get a call any minute.
When on trucks, we get no breaks. We do get plenty of downtime and honestly, I’m lucky to work in a system where we do get downtime. Also, we aren’t too, too busy, but inevitably you’re going to get calls.
Some days, there are, at least in southern Massachusetts, a lot of calls coming in because not a lot people seem to want to go to the hospital unless they absolutely have to. But now, they are not calling 911 unless it’s life or death. To an extent it’s good because A. it saves up the hospital beds for the hospitals since they are seeing the surges, and B. it’s good for patients now be more cognizant of the medical conditions. They can ask themselves, do I truly in need of ER or 911, or can I say call my personal physician first? Yeah. And then our shifts, depending on when it ends, we have downtime for up to 24 hours 36 sometimes when we are allowed to sleep.
TN: You can’t go back home, right? Is that what is going on?
MP: Can’t go back home. So, if you’re on shift you want to stay at the base for whoever longer shift, 12 24 36 hours, is over. Or you can go home, if you so choose. There is concerns obviously people not wanting to encounter their families and infect them. I can’t test that as much because I slept by myself in my apartment in Quincy. That’s not so much a problem.
TN: Is your family doing okay?
MP: My family’s doing okay. It seems that I’m the only one who’s really active in health care right now. Most of them are hunkered down in isolation at home. So, they always are asking me how I’m doing.
TN: So, one of my few last questions is how an SMS or 911 call might be different now as to the personnel respond to it. Knowing that there might be an additional danger beyond anything they might expect.
MP: I talked earlier about PPE, immensely preparing yourself. Now you go in, and you say, “Alright, what does this patient have?” And we’re trying to be more efficient. So, number one, it depends on if the patient’s truly sick, life threatening sick, like you were forced to act, if not, they’ll die versus are they managing okay by themselves as is. Also, because of this particular crisis, we don’t send everybody in all at once. In the past, we would have firefighters, police, and paramedics or EMTs show up, and we would all go in to make contact the patient. Now, especially with the high-risk patients, we’re trying to limit the number of people we have on them and limit the number of exposures. That’s one way we are trying to mitigate this.
Another way is just being more cognizant that we have all prepared with PPE, the danger lies in just the amount we have to actually physically interact with them only performing the assessments we absolutely need to perform. In the past, we did have some more flexibility to dig deeper if you’re really concerned about the underlying medical conditions patients. Now, with the pandemic, it’s very important to do what you have to do. But don’t go any further.
TN: How do you feel about that? I mean, not being able to send in all the troops to probably help someone.
MP: In the past before this, I thought that there were some calls where, you know, we didn’t need everybody there. You know, for instance, say we have, an individual who fell hurt their legs. That is not a too serious situation, but they might send the fire department and also the police there to assist, which is nice. Don’t get me wrong. I just didn’t feel it was totally necessary to have them there. You know, police officers have police calls to handle as well. Firefighters still have fire calls. However, those calls, I’m sure, makes a difference for them. And I respect that.
Now, it’s the threatening calls that concern me. You have the infectious patient in front of you now. It’s all hand on deck. They’re still there. Don’t get me wrong, they are still there when we need them. It just takes a few minutes to get them inside. But those patients are hard to handle. Yes, and sometimes the interventions you do to save them might expose yourself and others who don’t the protective equipment on.
TN: Yes, I guess that is just one of the dilemmas that we are all working to solve during this time. That’s all my question. Is there anything else you’d like to add?
MP: I guess the only thing I’d like to add is that it was a great per diem opportunity while at St. Lawrence University. I graduated in a positive light and SLU impacted who I am now, so I felt it was important to give back during these times.
TN: Thank you so much. I wish you all the best during this time.
MP: Thank you.



